Physiohtherapy after Childbirth
Congratulations, you have just given birth, are nearing your due date or you are just curious about what can happen to your body after childbirth and the role of a physio in your recovery.
You might have been made aware about these conditions by now, we will be talking through some of these common conditions that occur after childbirth that can often be overlooked and left untreated.
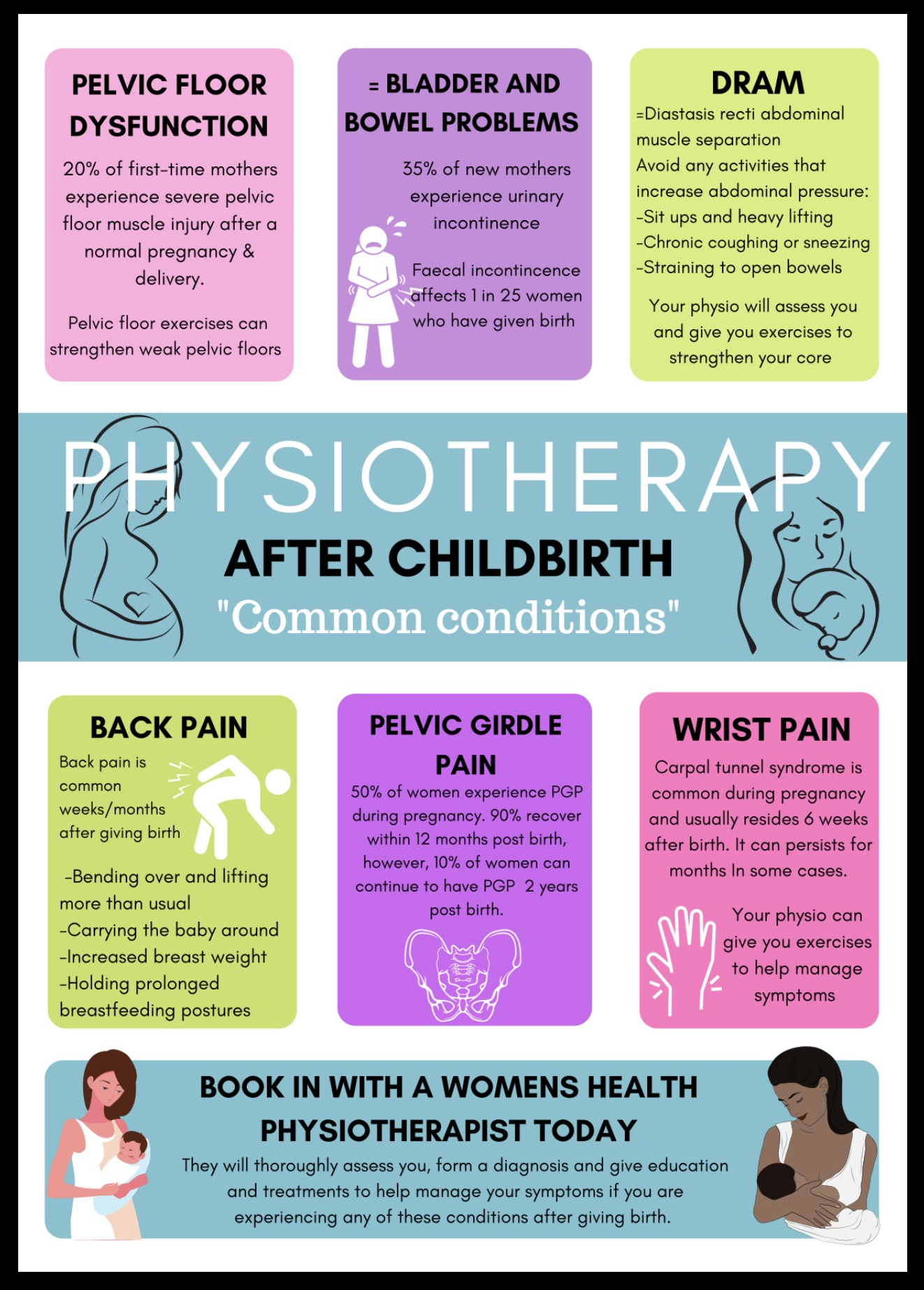
Pelvic floor disorders
The pelvic floor is located internally and consists of muscles, ligaments, fascia and nerves that allow for performance of basic everyday functions in males and females: keeping our pelvic organs in place, aiding in normal urination, defecation, and sexual function (Parezanovic-Ilic et al, 2017). Weakness or damage to the pelvic floor muscles (PFM) from pregnancy and childbirth (both vaginal and caesarean births) can result in pelvic floor disorders such as urinary incontinence, faecal incontinence and pelvic organ prolapse (Parezanovic-Ilic et al, 2017).
Treatment:
Research supports the use of PFM exercises in resolving or reducing urinary incontinence and other pelvic floor disorders (Haddow, Watts, & Robertson, 2005). Evidence shows that supervised PFM training programs (by a trained physiotherapist) are more successful than self-directed ones (Hay-Smith, Herderschee, Dumoulin & Herbison, 2011) as over 30% of people are unable to contract their PFM when first instructed (Benvenuti et al., 1987).
Book in with a women’s health physiotherapist today, they will create an exercise program for you. The program should last for at least 3 months to be most effective (Dumoulin & Hay-Smith, 2010).
Tips:
Imagine your PFM is shaped as a dome, and you are trying to bring the centre of it up, hold and then relax and bring it down.
Tense those PFM as if you’re stopping yourself from peeing mid-stream
Once you have the technique down pat, contract as hard as you can and hold for 3-10 seconds.
Repeat 10 times and try to do this 3-4 times per day eg. when stopped at the traffic lights
Always remember to keep breathing, don’t hold your breath
Make sure there is no movement at your butt as you should not be contracting the glutes
Try to relax your belly as we don’t want to be contracting your abdominal muscles either
TIPS: “Tense and release” “Up and down” “Contract and relax”
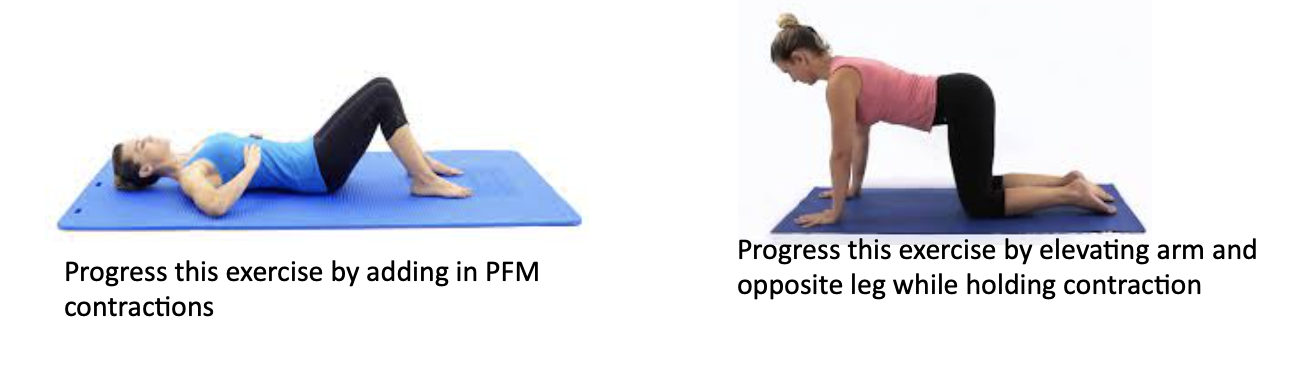
DRAM (Diastasis of the rectus abdominal muscle)
DRAM is the separation of the rectus abdominal muscle where the linea alba (connective tissue) widens during pregnancy and creates a gap.
A study found that DRAM was prevalent in 60% of women six weeks postnatal and remained prevalent in 32.6% of women 12 months’ postnatal (Sperstad, Tennfjord, Hilde, Ellström- Engh, & Bø, 2016).
A physiotherapist should check this for you, but it can also be done at home. Lie down on your back with your knees bent, place two fingers width ways 4.5cm above your belly button, raise your head and reach one arm towards feel to turn on those muscles and feel for a gap. Also measure 4.5cm below the belly bottom.
Treatment
A study by Benjamin et al (2014) found that exercises targeting the abdominal muscles, specifically the transversus abdominis muscle helps to reduce the width of DRAM separation.
Here are some exercises you can do at home
-Recreate the positions below.
-Draw belly button into spine
-Hold for 10 seconds and repeat 10 times, 3x daily
-Remember to breathe during these exercises
TIPS:
-Avoid activities which increase your abdominal pressure:
Sit ups
Heavy lifting
Chronic coughing or sneezing
Straining to open bowels
-Compression use (Tubi grip) around belly
-Education on correct postures and how to get out of bed properly (Side lie)
Musculoskeletal pain
Back pain is very common in the weeks/months after giving birth as new mothers are bending over and lifting more than usual, have increased weight in their breasts, holding prolonged breastfeeding postures and are generally feeling more fatigued.
TIPS:
Maintaining good posture when sitting/standing/walking
Avoiding lifting heavy things
Using chairs with good back support
Avoid holding baby on one hip
Getting a support belt
Using heat or icepacks for pain relief
Avoid prolonged sitting
Sleep side laying with a pillow between knees
Keep active, walking is good
Pelvic girdle pain (PGP) is pain over the pubic bone or buttocks and can radiate down the thighs. It can be more debilitating than low back pain (Walters, West. & Nippita., 2018).
TIPS: (Homer & Oats, 2018)
See a physiotherapist regarding exercise and posture
Wearing low heeled shoes
Reducing non-essential weight bearing activities (eg climbing stairs, standing/walking for long periods of time)
Use of pelvic support garments
Avoiding standing on one leg (eg sit down to get dressed)
Avoiding movements involving hip (getting in and out of car, baths and squatting)
Applying heat to painful areas
Wrist pain: Carpal tunnel syndrome (CTS) Is a common condition that occurs during pregnancy. A study by Mora et al (2018) found that although most symptoms decrease after 6 weeks post-partum, 15% of women still experienced persistent symptoms that worsened over time and lasted over 3 months post partem
CTS causes pain, weakness, numbness, pins and needles or a burning sensation in our hands and fingers.
By Sophie Chapman, Physiotherapy student at Exercise Thought
References:
Benjamin, D., van de Water, A., & Peiris, C. (2014). Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy, 100(1), 1-8. http://dx.doi.org/10.1016/j.physio.2013.08.005
Benvenuti, F., Caputo, G. M., Bandinelli, S., Mayer, F., Biagini, C., & Sommavilla, A. (1987). Reeducative treatment of female genuine stress incontinence. American journal of physical medicine, 66(4), 155–168.
Dehghan, F., Haerian, B. S., Muniandy, S., Yusof, A., Dragoo, J. L., & Salleh, N. (2014). The effect of relaxin on the musculoskeletal system. Scandinavian journal of medicine & science in sports, 24(4), e220–e229. https://doi.org/10.1111/sms.12149
Dumoulin, C., & Hay-Smith, J. (2010). Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. The Cochrane database of systematic reviews, (1), CD005654. https://doi.org/10.1002/14651858.CD005654.pub2
Haddow, G., Watts, R., & Robertson, J. (2005). Effectiveness of a pelvic floor muscle exercise program on urinary incontinence following childbirth. International journal of evidence-based healthcare, 3(5), 103–146. https://doi.org/10.1111/j.1479-6988.2005.00023.x
Hay-Smith, E. J., Herderschee, R., Dumoulin, C., & Herbison, G. P. (2011). Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women. The Cochrane database of systematic reviews, (12), CD009508. https://doi.org/10.1002/14651858.CD009508
Homer., C, & Oats., J. (2018). Clinical practice guidelines: Pregnancy care. Canberra: Australian Government Department of Health, p. 355–57. Retireved from https://www.health.gov.au/sites/default/files/pregnancy-care-guidelines_0.pdf
Mora, A., Blazar, P., Teplitz, B., Rogers, J., Economy, K., & Earp, B. (2018). Prospective Evaluation of the Incidence and Persistence of Gestational Carpal Tunnel Syndrome. The Journal Of Hand Surgery, 43(9), S9. doi: 10.1016/j.jhsa.2018.06.036
Parezanovic-Ilic, K., Mladenovic-Segedi, L., Jurisic-Skevin, A., Zivanovic-Macuzic, I., Grbovic, V.,
Nurkovic, J., Jovanovic, M., & Jeremic, D. (2017). The influence of various risk factors on the strength of pelvic floor muscle in women. Vojnosanitetski pregled, 74(6), 557-563. doi: 10.2298/VSP150420083P
Sperstad, J., Tennfjord, M., Hilde, G., Ellström-Engh, M., & Bø, K. (2016). Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. British Journal of Sports Medicine, 50(17), 1092-1096. Retrieved from http://dx.doi.org/10.1136/bjsports-2016-096065
Walters., C, West., S., & Nippita., T. (2018). PELVIC GIRDLE PAIN IN PREGNANCY. AJGP VOL. 47, NO. 7, P 439-443. Retrieved from https://dbb715huzqn8k.cloudfront.net/e4/2d/e42d98eaf8ff6ce6eb49a7f578a7fac6ca5402fd?response-content-disposition=inline%3Bfilename%3D%22Pelvic%20pain%20in%20pregnancy%20Nippita%20et%20al%202018%20.pdf%22&responsecontenttype=application%2Fpdf&Expires=1628169428&Signature=FVTjtpISF7WglhQRB9WNJ2xZ5F52vXdO7SpC8DgrS4RNGdAs0YcLurfDt5~UwpmTBpnlJ7iFuzR1bdpZvSm5Pbj4jC8b8PorD7fjbwYFYm-EfDWC7CzAOX8ZMMARaO6RyoPy-K8R~Kx5JKJmFplBgPnYz9QpXEqUt1UERr3YJNjhnjd97BlmOS3cALzeIXMHSJehfZ4B8zF9bSYOdoPKaZ9uApTSOYRmMvVKyTzOK4vl7bF6Tl20p4-jddDEbE5u3jAtkCPZERFPeFlb~3AxHGw-0e-l5zh5gBS~PglbpBddu9ebHSkoHitz9-U3bAobymVq0WUc-eb8HtidnmIB0g__&Key-Pair-Id=APKAJMYMTS3PZ4IMRVZQ