Physiotherapy for Fibromyalgia
Fibromyalgia Is a condition that causes widespread pain all over the body and results in sleep problems, fatigue and emotional and mental distress. The causes are unclear however it is not an autoimmune or inflammation-based disease. Current research demonstrates involvement from the central nervous system (American College of Rheumatology, 2021). More recently, Fibromyalgia has been described as Central Pain Amplification disorder, meaning the volume of pain sensation in the brain is turned up too high.
Fibromyalgia is associated with decreased quality of life, higher rates of major depression, higher rates of osteoarthrosis, rheumatoid arthritis and is linked to more hospitalisations, 2x more than a person without fibromyalgia (Centre for Disease Control and Management, 2020).
Common signs and symptoms:
Increased sensitivity to pain
Pain and stiffness all over the body in the muscles and joints
Fatigue and tiredness
Sleep problems
Depression and Anxiety
Headaches and migraines
Problems with memory and concentration, brain “fogginess”
Other symptoms could include:
-Pins and needles or numbness in the hands and feet
-Pain in the face or jaw including jaw disorders like temporomandibular joint syndrome (TMJ)
-Digestive problems, including bloating, abdominal pain, constipation, and irritable bowel syndrome (IBS)
(Centre for Disease Control and Management, 2020).
Fibromyalgia affects 2% of the Australian population with a peak prevalence in middle aged women (Kwiatek, 2017).
Risk Factors:
Age. Fibromyalgia can affect all ages however you are more likely to have fibromyalgia as you get older (Middle age).
Lupus or Rheumatoid Arthritis. If you have lupus or rheumatoid arthritis (RA), you are more likely to develop fibromyalgia.
Some other possible factors:
Females are twice as likely to have fibromyalgia as Males.
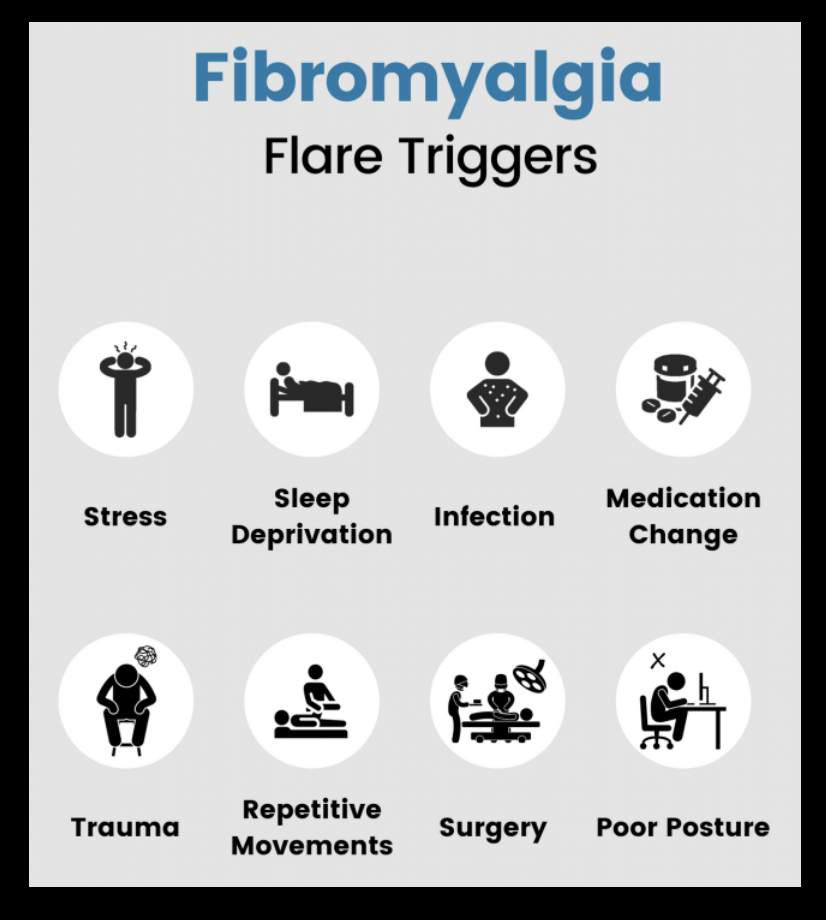
Stressful or traumatic events, such as car accidents, post-traumatic stress disorder (PTSD)
Repetitive injuries. Injury from repetitive stress on a joint, such as frequent knee bending.
Illness (such as viral infections)
Family history
Obesity
(Centre for Disease Control and Management, 2020).
Diagnosis:
A doctor or rheumatologist usually diagnoses you. They look at your medical history, can do blood tests. There are no specific tests or imaging to diagnose fibromyalgia, however your doctor may conduct specific tests to rule out other conditions.
A patient satisfies diagnostic criteria for fibromyalgia if the following 3 conditions are met:
1.Widespread pain index (WPI)
2. Symptoms have been present at a similar level for at least 3 months.
3.The patient does not have a disorder that would otherwise explain the pain.
Treatment:
A multidisciplinary approach is the best treatment strategy for Fibromyalgia. The most beneficial treatments are individualised and consist of nutrition education, address sleep, medicine, exercise, and psychological treatments that focus on mood management and positive coping strategies (Offenbächer & Stucki, 2000).
Managing fatigue:
Symptoms can fluctuate meaning that you can have good days and bad days. Overdoing it can lead to exacerbated symptoms the next day, so it is important to know your limitations and triggers.
Pacing your activities throughout the day is a good technique to manage your fatigue and save your energy.
Stress and Anxiety
Having healthy coping strategies is important.
Do what works for you, listening to music, going for a walk, meditation, mindfulness, positive affirmations, yoga and so on.
If stress is overwhelming, talking to a psychologist could help in developing strategies to help cope with stressful situations.
Sleep health:
Understanding sleep and its influence on health are vital in helping people who have Fibromyalgia. Poor sleep health can affect your mood, brain function, emotions, muscle recovery, immune system, nervous system, and your hormones.
Some tips for a good night sleep include:
Having a hot shower
Disconnect from devices before bed
Doing some meditation or listening to meditation sounds, the ocean or rain sounds
Calming scents like Lavender through diffusers or room sprays
Decrease caffeine consumption later in the day
Reduce irregular or long daytime naps
No alcohol consumption at night
Don’t eat too late
Exercise regularly but not right before bed
Optimise bedroom environment and reduce lighting in your room
Melatonin supplements
Try to sleep at consistent times
(Sleep foundation, 2020)
Physiotherapy for Fibromyalgia:
You can see a physiotherapist if exercise is new to your lifestyle as some exercise can exacerbate symptoms. It is important to work closely with a physiotherapist who can monitor the effect of the interventions and your symptoms to give you the best exercise program suited to you (Australian physiotherapy association, 2021).
Physiotherapists can create exercise programs, provides massages, acupuncture, joint mobilisation and other physical therapies. Aerobic and muscle strengthening exercises are the most effective way of reducing pain and improving global well-being in people with fibromyalgia (Sosa-Reina et al, 2017). Stretching and aerobic exercises also increases health-related quality of life in people living with fibromyalgia.
Another study by Busch et al. (2013) found that moderate and moderate to high-intensity resistance training improves multidimensional function, pain, tenderness, and muscle strength in women with fibromyalgia.
Physiotherapy treatment will be individualised based on personal symptoms and functional limitations. Book in will your local physio today If you are eager to commence an exercise program.
By Priya Narayan, Physiotherapy Student at Exercise Thought
References:
American College of Rheumatology. (2021). Fibromyalgia. Retrieved from https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Fibromyalgia
American College of Rheumatology. (2010). Fibromyalgia diagnostic criteria. Retrieved from
https://www.rheumatology.org/portals/0/files/2010%20fibromyalgia%20diagnostic%20criteria_excerpt.pdf
Australian physiotherapy association. (2021). Choose physio: for Fibromyalgia. Retrieved from https://choose.physio/your-condition/fibromyalgia
Busch, A. J., Webber, S. C., Richards, R. S., Bidonde, J., Schachter, C. L., Schafer, L. A., Danyliw, A., Sawant, A., Dal Bello-Haas, V., Rader, T., & Overend, T. J. (2013). Resistance exercise training for fibromyalgia. The Cochrane database of systematic reviews, 2013(12), CD010884. https://doi.org/10.1002/14651858.CD010884
Centre for Disease Control and Management. (2020). Arthritis: Fibromyalgia. Retrieved from
https://www.cdc.gov/arthritis/basics/fibromyalgia.htm#what
Kwiatek, R. (2017). Treatment of fibromyalgia. Aust Prescr, 40:179-83. Retrieved from https://doi.org/10.18773/austprescr.2017.056
Offenbächer, M., & Stucki, G. (2000). Physical therapy in the treatment of fibromyalgia. Scandinavian journal of rheumatology. Supplement, 113, 78–85. https://doi.org/10.1080/030097400446706
Sleep foundation. (2020). Healthy sleeping tips. Retrieved from https://www.sleepfoundation.org/sleep-hygiene/healthy-sleep-tips
Sosa-Reina, M. D., Nunez-Nagy, S., Gallego-Izquierdo, T., Pecos-Martín, D., Monserrat, J., & Álvarez-Mon, M. (2017). Effectiveness of Therapeutic Exercise in Fibromyalgia Syndrome: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. BioMed research international, 2017, 2356346. https://doi.org/10.1155/2017/2356346