Osgood Schlatter’s Disease
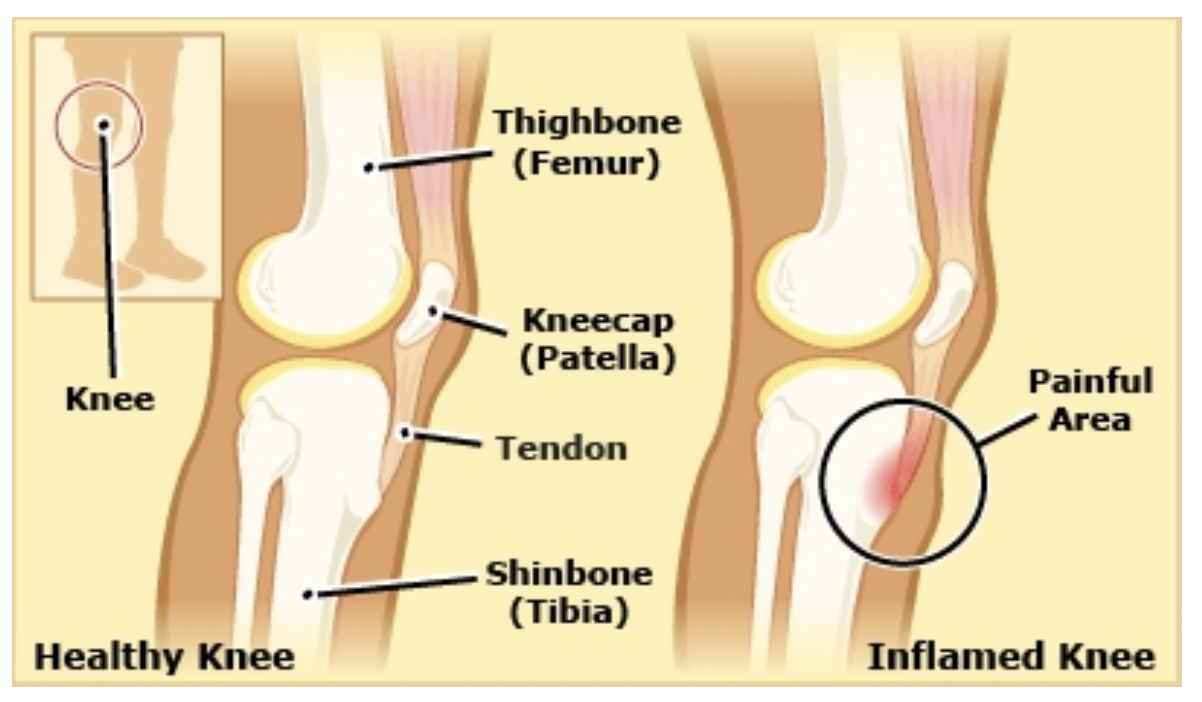
Osgood Schlatter Disease (OSD), commonly known as ‘growing pain’, is a common complaint at the front side of the knee(s) among active 10–15-year-old children. Symptoms often arise in activities such as jumping, running, squatting and kicking (Ladenhauf et al., 2020).
What causes OSD?
The exact cause of OSD is unknown, however there are several theories as to why it may occur. The two most prominent theories are:
Inflammation due to repeated grinding of the patella tendon against the upper part of the tibia (shin bone). This leads to avulsion fractures, where a small chunk of bone attached to the tendon gets pulled away from the main part of the bone, leading to pain and swelling.
Changes in the patella tendon and surrounding structures cause the child pain and swelling in the area.
What factors contribute to having OSD?
There are a few known modifiable and non-modifiable risk factors:
Non-modifiable factors include:
male gender
Patellofemoral alignment (how the kneecap and thigh bone align)
stage of physeal growth (portion of bone that can grow)
Modifiable factors include:
a higher body weight and/or BMI
weekly practice routine
tightness of the hamstrings, calf, and quadriceps
reduced core stability
(Ladenhauf et al., 2020)
Is an X-ray needed to confirm OSD?
The diagnosis could rely solely on a thorough history and examination by a physiotherapist; thus, an x-ray is often not required. An X-ray to exclude possible free ossicles and further rule-out other conditions.
What should I expect from a consultation with a physiotherapist?
Physiotherapists will look out for a few key indicators. They may commence with identifying activities involving extensive knee loading. As we mentioned at the beginning of the article, this may include activities such as jumping, running, squatting and kicking. Physiotherapists may look and feel for possible thickening and tenderness of the patella tendon and assess the complete lower extremity for muscular weakness and tightness.
Treatment
Treating OSD currently relies on mostly clinical reasoning and expert opinion since we do not have a lot of data. Recommended strategies include activity modification, pausing provocative activities, exercises, flexibility training of tight muscles, core stability training, NSAID’s to manage pain and/or ice to manage swelling. Rathleff et al (2020) suggested exercises to strengthen the musculature surrounding the knee and hip joint. These included isometric leg extensions (Figure 1), wall squats (Figure 2), bodyweight squats (Figure 3), lunges (Figure 4), and hamstring bridges (Figure 5) (Rathleff et al., 2020).
Figure 1: Isometric leg extensions with towel under knee
Figure 2: Wall squat
Figure 3: Bodyweight squat
Figure 4: Lunges
Figure 5: Hamstring bridges
Corticosteroid injections are not recommended (Circi et al., 2017; Nehaus et al., 2021). Consult a physiotherapist to discuss your options to work besides you to make a more informed decision.
By Omer Turkmen, student at Exercise Thought.
References
Circi, E., Atalay, Y., & Beyzadeoglu, T. (2017). Treatment of Osgood–Schlatter disease: review of the literature. Musculoskeletal surgery, 101(3), 195-200.
Ladenhauf, H. N., Seitlinger, G., & Green, D. W. (2020). Osgood-Schlatter disease: a 2020 update of a common knee condition in children. Current opinion in pediatrics, 32(1), 107–112. https://doi.org/10.1097/MOP.0000000000000842
Neuhaus, C., Appenzeller-Herzog, C., & Faude, O. (2021). A systematic review on conservative treatment options for OSGOOD-Schlatter disease. Physical Therapy in Sport.
Rathleff, M. S., Winiarski, L., Krommes, K., Graven-Nielsen, T., Hölmich, P., Olesen, J. L., Holden, S., & Thorborg, K. (2020). Activity Modification and Knee Strengthening for Osgood-Schlatter Disease: A Prospective Cohort Study. Orthopaedic journal of sports medicine, 8(4), 2325967120911106. https://doi.org/10.1177/2325967120911106